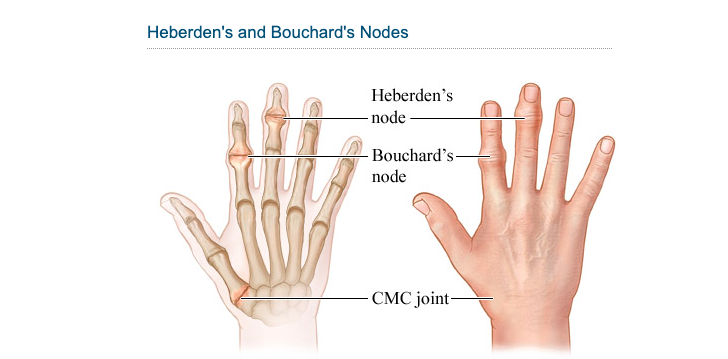
Bouchard’s nodes are bony protrusions on the knuckles, middle joints, and other flexed digits. Your proximal interphalangeal joints are the ones closest to your hand. Symptoms of Bouchard’s nodes include a lack of mobility, swollen and stiff joints, weakness, and crooked fingers. Any number of your fingers is susceptible to developing Bouchard’s nodes. We speak about Heberden’s nodes when they appear on the distal phalangeal joints. Rarely seen lymph nodes called Bouchard’s are linked to severe forms of arthritis. The differentiation between osteoarthritis and psoriatic arthritis in the finger joints is one of the most difficult diagnostic issues. Here we will discuss more of Bouchard’s nodes in detail.
Where do Bouchard’s nodules come from?
When the cartilage that separates the bones in your fingers goes away, a condition known as Bouchard’s nodes develops. This cartilage reduces the amount of wear and tear on your joints. Bones start to rub against each other as it wears out. This may cause joint injury and lead to bone growth. New bone growth can cause crooked fingertips. Age, previous injury, a job requiring hand movement, and a family history of Bouchard’s nodes are risk factors for hand osteoarthritis.
Joint inflammation caused by psoriasis:
Several symptoms, including joint pain, oedema, and stiffness, characterize psoriatic arthritis. Psoriatic arthritis affects approximately one-quarter of patients who have psoriasis. Psoriatic arthritis often manifests itself between 5 and 10 years following the initial diagnosis of psoriasis. Psoriasis patients may also be at risk for developing other types of arthritis, such as osteoarthritis, which can make an accurate diagnosis difficult.
When comparing psoriatic arthritis to osteoarthritis?
Damage to the cartilage lining your joints, brought on by constant usage, is the root cause of osteoarthritis. When your immune system mistakenly attacks healthy cells, it causes joint damage, known as psoriatic arthritis. Psoriasis is linked to both rheumatoid and psoriatic arthritis. Psoriatic arthritis’s aetiology remains a mystery. People with psoriatic arthritis are more likely to have a first-degree relative with either psoriasis or psoriatic arthritis, with the prevalence varying between 30 and 50 per cent, depending on the study. The average age of onset is between 30 and 50.
Symptoms of psoriatic arthritis:
Stiffness, swelling, discomfort, pitting or splitting of the nails, and scaly patches on the skin are all possible symptoms of arthritis. However, their severity depends on the affected joint. Periods of increased symptom severity, or “flare-ups,” are possible. Some people’s joint pain is severe and affects several joints, while others may only have modest discomfort in one or two joints.
Osteoarthritis:
Age increases the prevalence of osteoarthritis, the most prevalent form of arthritis. Almost 80% of the senior population in the United States displays symptoms of osteoarthritis. Joint wear and tear over many years is the root cause of osteoarthritis. In most cases, it manifests gradually and worsens as the joint sustains more injury. Treatment may alleviate some of the discomfort associated with osteoarthritis, but there is no cure.
Psoriatic arthritis affects the hands:
Psoriatic arthritis frequently affects the hands in its course of progression. There is also a possibility of the condition occurring in the knees, ankles, and feet. The symptoms of hand psoriatic arthritis are similar to those of other types of the illness. Patients may experience heat emanating from the affected joint, redness, oedema, a reduced range of motion, and stiffness. One of your hands may react differently to the effect than the other.
Medications:
Your doctor could recommend capsaicin or other NSAIDs as a course of therapy. In cases like these, it’s best to listen to your medical professional’s advice. As you can see, these are only a handful of the many possible options. It’s a small sample of the many more out there. Many different product forms may be appropriate for therapeutic usage. We can’t rule out the potential of this happening. Numerous dosage forms, such as capsules, creams, and lotions, are readily accessible.
Making adjustments to one’s motions and motion patterns:
If you modify your hand movements and stop doing the things that are aggravating the pain, you should feel better soon. Alternatives to continuing to use the same activities that irritate your hands include changing how you use your hands and stopping using those same actions altogether. Using this approach may relieve some of the stress that has been building up in your hands. If you can strictly adhere to these instructions, you may find relief from your current predicament.
Extremes in temperature:
Some individuals relieve joint discomfort after applying heat to the area, while others find it more helpful to apply ice. When medical interventions like medication and other non-invasive therapies have failed to alleviate your illness, your doctor may suggest invasive surgical procedures as an additional option. Surgery for hand arthritis is seldom done because of the significant risk of complications and the large probability that the treatment will not be successful.
Osteoarthritis of the hand:
A possible aid in distinguishing between the two is the presence of Bouchard’s nodes, which are a prevalent factor in the onset of osteoarthritis of the hand. The afflicted patient’s palm contains these lymph nodes. Charles-Joseph Bouchard, a renowned French surgeon, was the source for their given and family names. Sometimes the hands and palms of people with psoriatic arthritis seem dry, cracked, and scaly, with a reddish hue. These symptoms may be caused, in part, by psoriatic arthritis.
How often are Bouchard’s nodes in arthritis?
Bouchard’s nodes indicate osteoarthritis of the finger joints, not psoriatic arthritis, as is often believed. They are easy to spot because the bones around the joint where two fingers connect protrude in that direction. The presence of these bumps enables medical professionals to distinguish osteoarthritis from other types of arthritis. Your physician will most likely recommend a more conservative treatment, such as reducing the amount of physical activity you engage in or using non-steroidal anti-inflammatory medicines.
Conclusion:
Bouchard’s nodes are a symptom of osteoarthritis of the finger joints, not psoriatic arthritis, as is often believed. They are visible as protrusions of bone around the joint where two fingers meet. These bumps help doctors identify osteoarthritis as opposed to other forms of arthritis. Pain from arthritis in the hands is real, but there are ways to alleviate it with the aid of your doctor. A surgical procedure may be suggested if they don’t help with your pain.
FAQs:
What are Bouchard’s nodes?
The nodules seen in Bouchard’s syndrome are an indicator of osteoarthritis. In spite of the fact that its origin is unknown, osteoarthritis is generally understood to be the result of years of joint usage.
How do you repair Bouchard’s nodes?
Bouchard’s nodes may be treated with bed rest, cold or heat packs, pain medications, or steroid injections when discomfort is present. Therapy for the hands may reduce the risk of impairment and improve mobility in arthritic or injured joints.
Can you describe the appearance of a Bouchard’s node?
Bony lumps on the middle knuckles of your fingers are the primary indicator of advanced OA and a diagnosis of Bouchard’s nodes.